Stroke Care
Blood Clot Prevention in Hospital
What are we measuring?
We measure the percentage of Ischemic or Hemorrhagic stroke patients who received treatment to keep blood clots from forming anywhere in the body within two days of hospital admission.
Why is it important?
Stroke patients are at an increased risk of developing venous thromboembolism (VTE). Reported rates of occurrence vary depending on the type of screening used. Prevention of VTE, through the use of prophylactic therapies, in at risk patients is a noted recommendation in stroke clinical practice guidelines.
How do we maintain compliance?
We are routinely educating staff on the use of customized order sets and documentation. An electric health record (EHR) has helped us to improve this.

Stroke Prevention Medicine at Discharge
What are we measuring?
We measure the percentage of Ischemic stroke patients who received a prescription for stroke prevention medication at discharge.
Why is it important?
Stroke prevention medication (antithrombotic) should be prescribed at discharge following TIA or acute ischemic stroke to reduce stroke recurrence, mortality and morbidity as long as no contraindications exist.
How do we maintain compliance?
We encourage use of neurology customized order sets and the use of stroke template for physician documentation, which requires this measure to be addressed.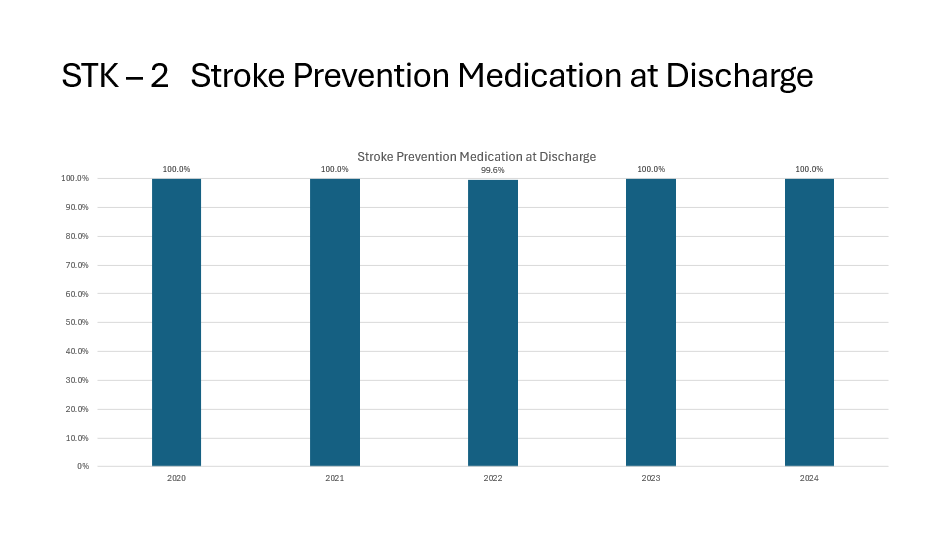
Blood Thinner Medicine at Discharge
What are we measuring?
We measure the percentage of Ischemic stroke patients with a type of irregular heartbeat who were given a prescription for a blood thinner at discharge.
Why is it important?
The administration of blood thinner medication (anticoagulation), unless there are contraindications, is an established effective strategy in preventing first or recurrent stroke in high stroke risk-atrial fibrillation patients with TIA or prior stroke.
How do we maintain compliance?
We encourage the use of stroke template for physician documentation, which requires this measure to be addressed.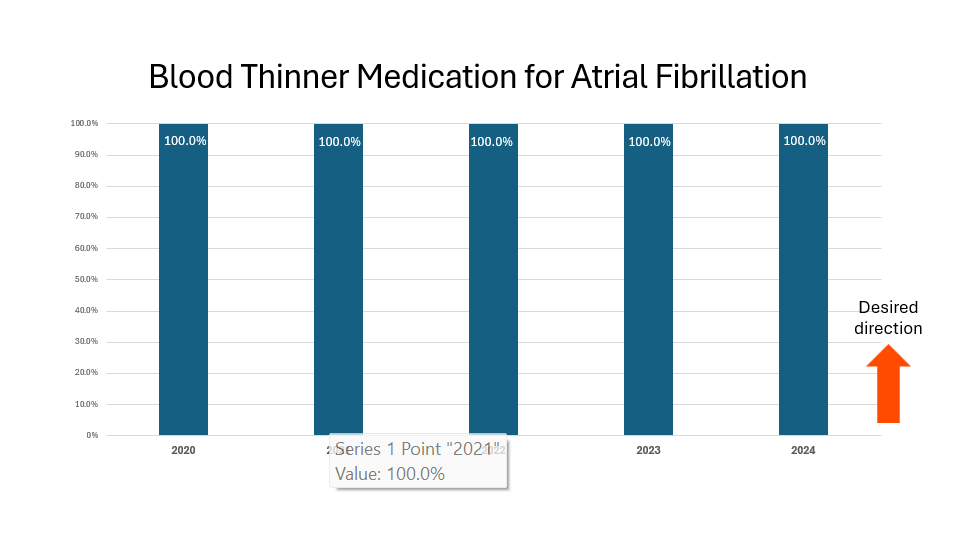
Clot-Busting Medicine in Hospital
What are we measuring?
We measure the percentage of Ischemic stroke patients who received clot buster medication within three hours of stroke symptoms starting.
Why is it important?
The earlier that clot buster medication (IV thrombolytic) is initiated, the better the patient outcome is. Guidelines support giving the clot buster drug up to 4.5 hours after symptom onset. Clot buster medication can be beneficial in improving function and minimizing or halting stroke damage.
How do we maintain compliance?
Summa encourages EMS to activate stroke alerts prior to emergency department arrival. We also provide ongoing education to Emergency Department staff for early recognition of stroke-like symptoms.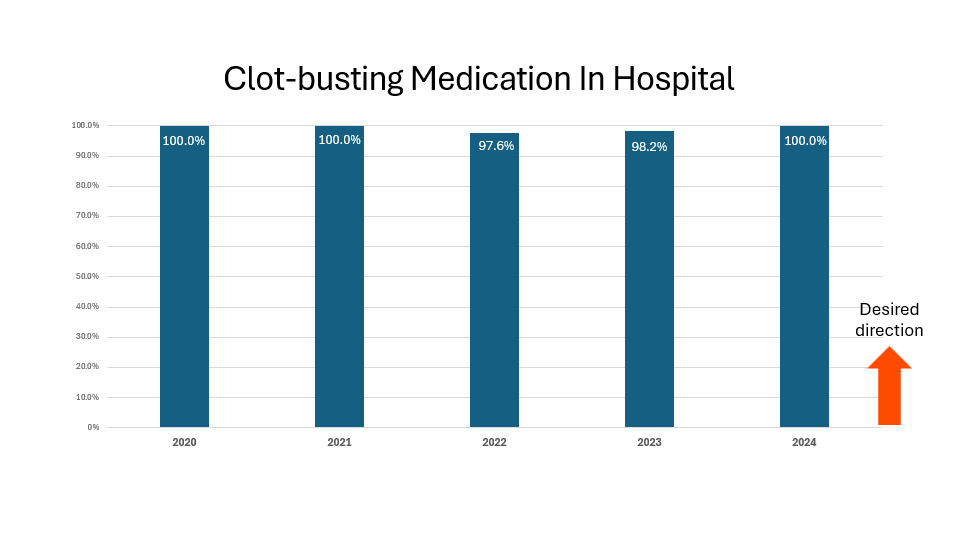
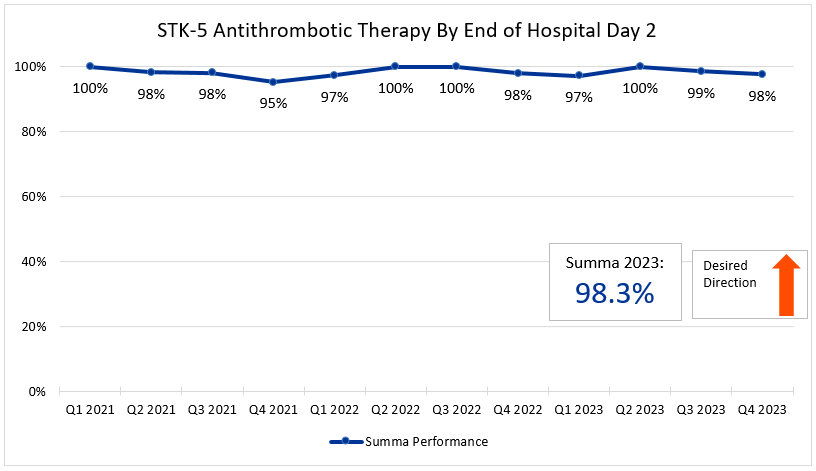
Stroke Prevention Medicine in Hospital
What are we measuring?
We measure the percentage of Ischemic stroke patients who received medicine for stroke treatment within two days of hospital admission.
Why is it important?
Data at this time suggests that antithrombotic therapy should be administered within two days of symptom onset in acute ischemic stroke patients to reduce stroke mortality and morbidity, as long as no contraindications exist.
How are we working to improve?
Summa encourages the use of neurology customized stroke order sets which require this measure to be addressed. And electronic health record has helped us to improve this.
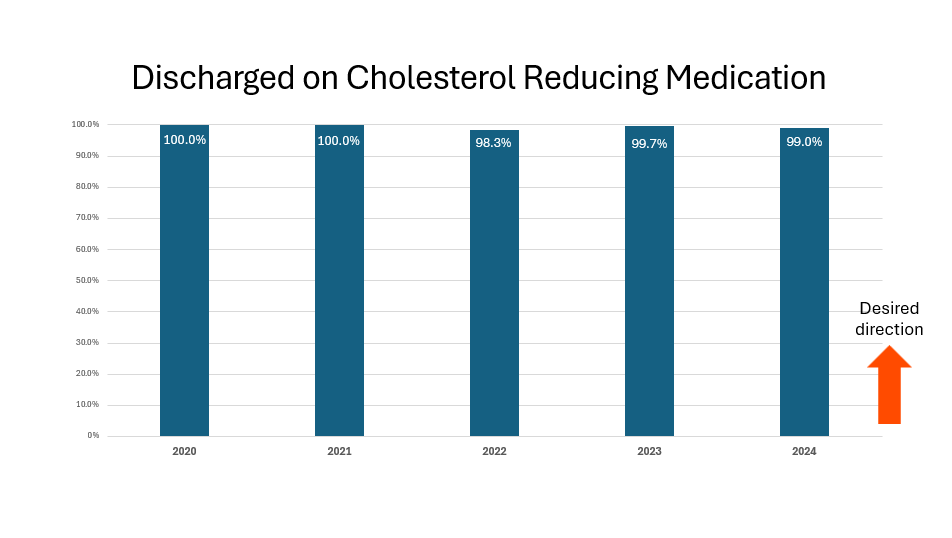
Cholesterol Medicine at Discharge
What are we measuring?
Some stroke patients are identified as having high cholesterol. We measure the percentage of stroke patients that are prescribed medication to help lower their cholesterol levels when leaving the hospital.
Why is it important?
Intensive lipid lowering therapy using statin medication (cholesterol medication) has been associated with a dramatic reduction in the rate of recurrent ischemic stroke and major coronary events. Intensive lipid lowering therapy through the use of a statin medication is recommended by stroke clinical practice guidelines.
How do we maintain compliance?
Updated stroke order sets to include intensive statin dosing. Physician use of a stroke template requires documentation of this measure. An electronic health record has helped us to improve as well.
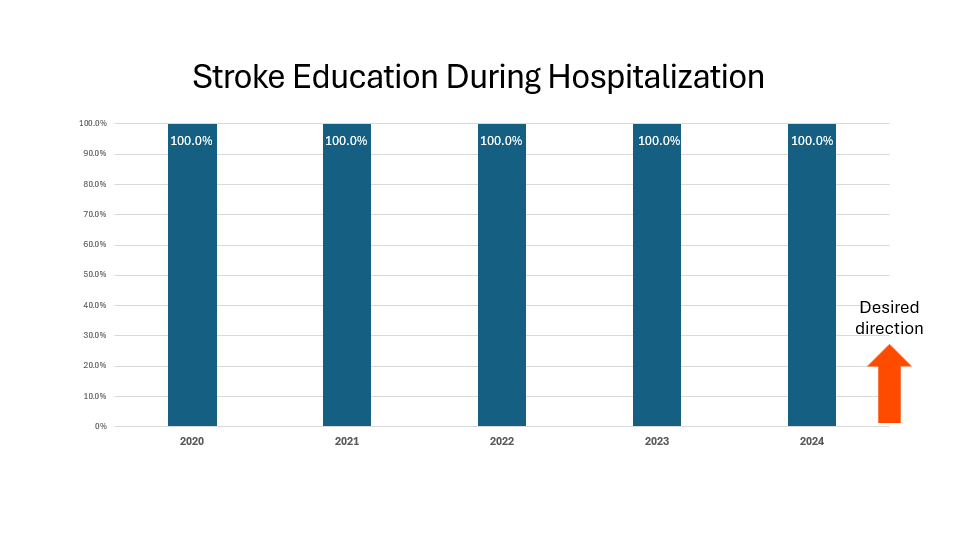
Stroke Education Materials
What are we measuring?
We measure the percentage of Ischemic or Hemorrhagic stroke patients or their caregivers who were given educational materials during the hospital stay addressing all of the following:
- Activation of an emergency medical system
- Need for follow-up after discharge
- Medications prescribed at discharge
- Risk factors for stroke
- Warning signs and symptoms of stroke
Why is it important?
There are many examples of how patient education programs for specific chronic conditions have increased healthful behaviors, improved health status, and/or decreased health care costs of their participants.
How do we maintain compliance?
Use of SMARTphrase for nursing to document required stroke education information. Daily audits of nursing documentation, providing immediate feedback.
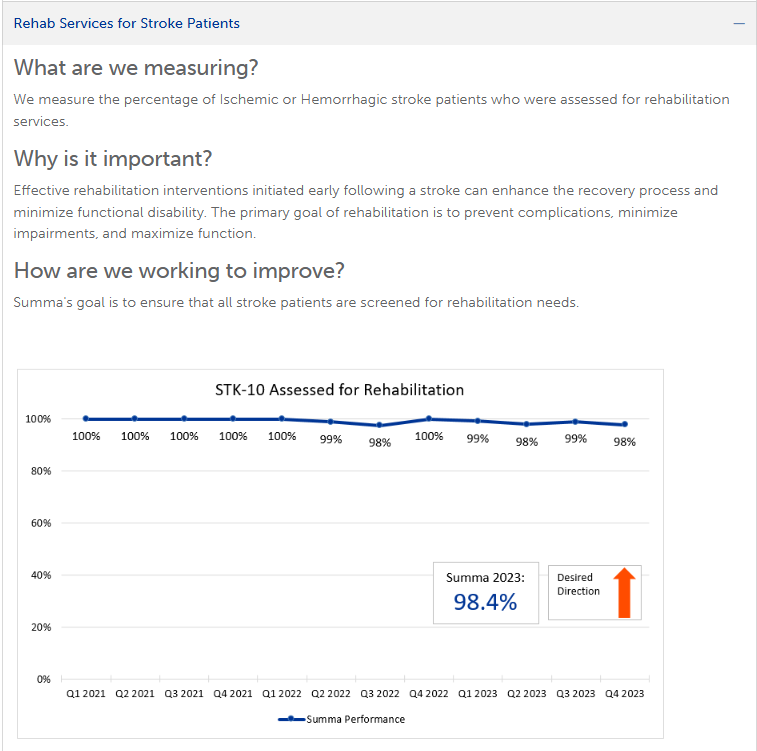
Rehab Services for Stroke Patients
What are we measuring?
We measure the percentage of Ischemic or Hemorrhagic stroke patients who were assessed for rehabilitation services.
Why is it important?
Stroke is the leading cause of serious, long-term disability. Effective rehabilitation interventions initiated early following a stroke can enhance the recovery process and minimize functional disability. The primary goal of rehabilitation is to prevent complications, minimize impairments, and maximize function.
How do we maintain compliance?
Summa's goal is to ensure that all stroke patients are screened for rehabilitation needs.
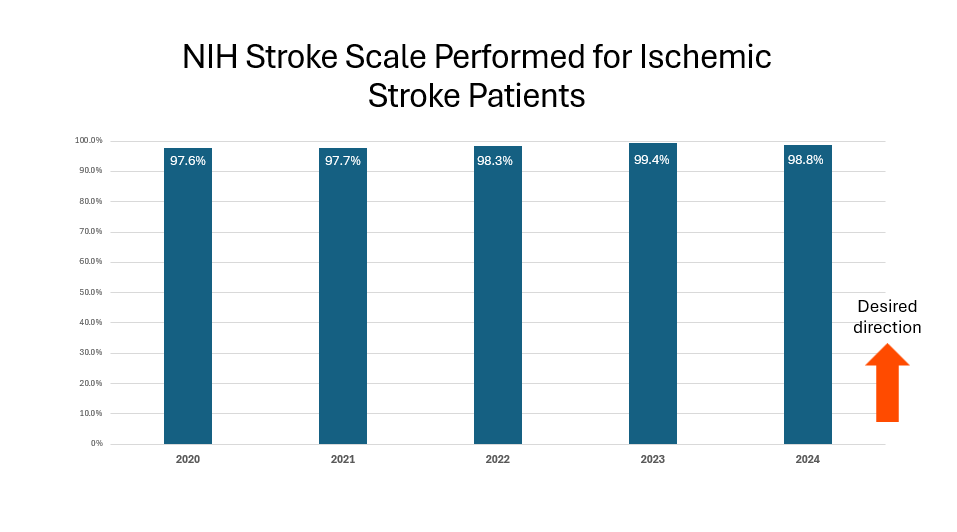
NIHSS Performed for Ischemic Stroke Patients
What are we measuring?
Ischemic Stroke patients for whom an initial National Institutes of Health Stroke Score (NIHSS) is performed prior to any acute stroke treatment or within 12 hours of arrival.
Why is it important?
A neurological assessment for all patients presenting to the hospital with signs & symptoms of stroke should be performed in a timely manner. The NIHSS is the preferred scoring tool recommended by the American Heart Association / American Stroke Association. Scores aid in the initial diagnosis of the patient, facilitate communication among healthcare professionals, and identify patients that may be eligible for treatment interventions or potential for complications.
How do we maintain compliance?
We are working with Emergency Department providers and nurses to standardize this assessment score into the electronic medical record template for all patients presenting with stroke like symptoms. All nurses on stroke units are NIH certified.
Time to Thrombectomy Procedure
What are we measuring?
We measure the median time from patient arrival in the emergency department to the start of clot retrieval procedure (skin puncture).
Why is it important?
Clot retrieval procedures are now standard of care for acute ischemic stroke treatment due to blockage of large blood vessel in the brain by a clot.
Timely restoration of blood flow is effective in reducing long-term disability. Earlier treatments are associated with increased benefits. National Goal is less than 90 minutes after emergency department arrival.
How are we performing?
In 2023, Summa's average time to procedure was 86 minutes which outperforms the national goal of 90 minutes.
How are we working to improve?
We review every thrombectomy case for potential ways of improving our communication and speed of treatment.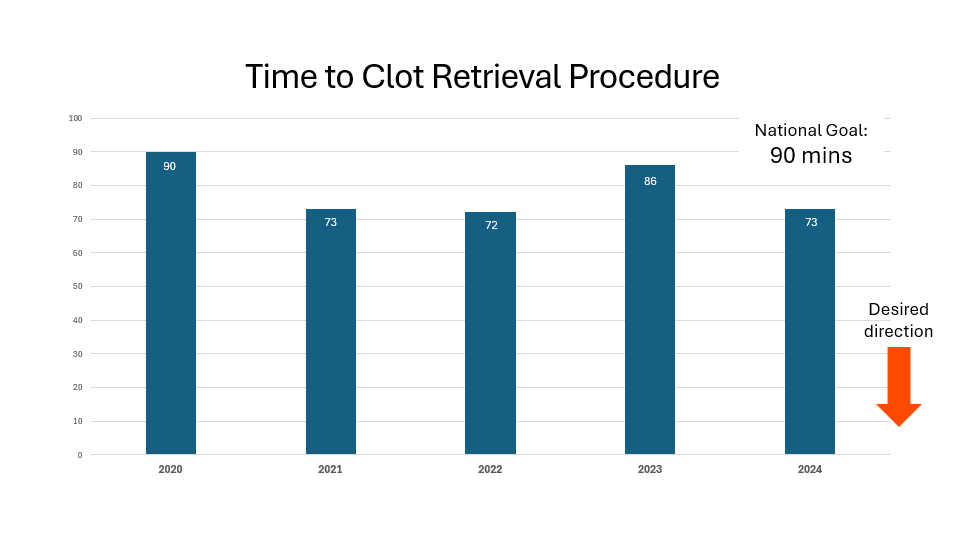
Intervention Complications
What are we measuring?
We measure types of bleeding complications within 36 hours of clot busting drug or mechanical clot retrieval procedures for acute stroke treatment.
Why is it important?
Bleeding is the most common risk after these treatments. Although rare, if bleeding in the brain occurs, the stroke could worsen and even be life threatening. A major trial found that 6.4% of patients treated with IV thrombolytic experienced symptomatic bleeding.
How are we performing?
In 2023, Summa's complication rate for bleeding was 2.2% which outperformed the National Goal of 6.0%.
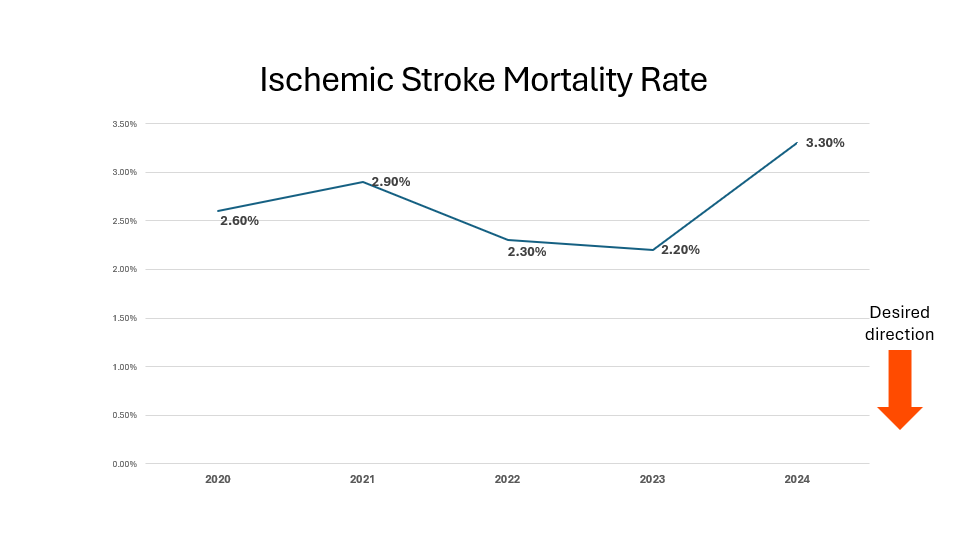
Ischemic Stroke Mortality Rate
What are we measuring?
We measure the mortality rate among acute care inpatient encounters with a diagnosis of ischemic stroke.
Why is it important?
As the highest level of stroke certification, Summa Health receives the most complex cases transferred for other hospitals.
Some deaths are expected in a hospital. However, we want to make sure we always provide the best care we can to minimize the number of people who die in our hospitals.
How do we remain compliant?
We monitor and review outcomes monthly. We consult palliative/hospice care when appropriate.
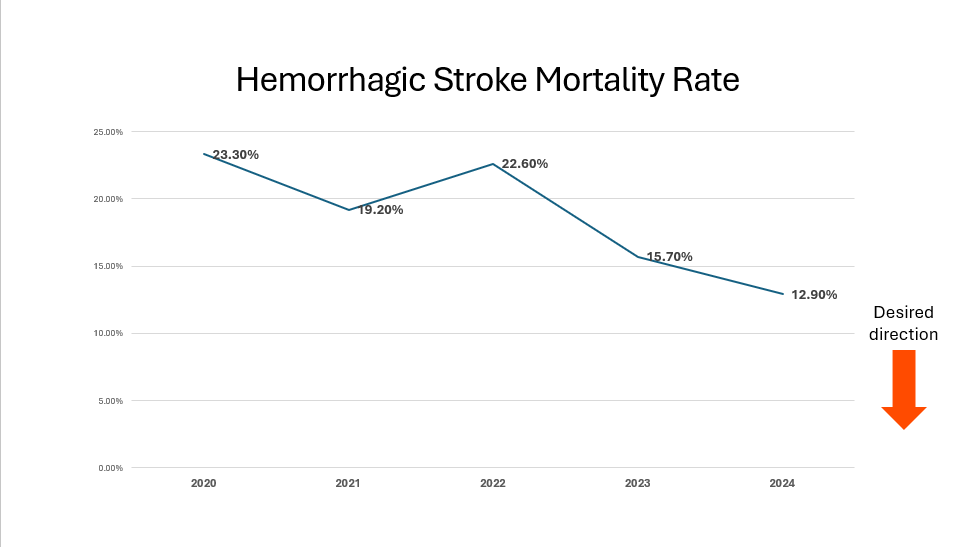
Hemorrhagic Stroke Mortality Rate
What are we measuring?
We measure the mortality rate among acute care inpatient encounters with a diagnosis of hemorrhagic stroke.
Why is it important?
Neurocritical care, neurosurgery and neurointerventional providers work collaboratively to treat and individualize care to the most complex types of stroke cases.
Some deaths are expected in a hospital. However, we want to make sure we always provide the best care we can to minimize the number of people who die in our hospitals.
How do we remain compliant?
We monitor and review outcomes monthly. We consult palliative/hospice care when appropriate.